As veterinarians, we love seeing our patients, but the feeling isn’t always mutual. For our patients, a visit to the veterinary clinic means encountering strange sights, sounds, and surroundings alongside the stress of being restrained and undergoing uncomfortable or potentially painful procedures. Low-stress handling techniques can make a big difference in how they experience care.
When our patients are anxious, our job becomes more difficult, too. It’s harder to interpret physiological parameters and perform a thorough physical examination, and anxiety and fear can lead to aggressive behavior that puts the veterinary team at risk.
Alleviating as much fear and anxiety as we can is crucial. This article outlines 4 steps you can take to manage anxiety and fear in your patients1: recognizing signs of stress, creating a low-stress clinic environment, practicing low-stress handling, and administering antianxiety medications before veterinary visits.
1. Learn to Recognize Signs of Stress and Fear in Dogs and Cats
Ensuring that veterinary team members are able to recognize signs of anxiety in dogs and cats is a vital first step, especially as signs can be subtle and easily missed.
Signs of Stress in Dogs and Cats
While some signs of stress in dogs and cats are fairly obvious, others can be harder to spot. This list covers the common signs, but keep in mind that patients probably won’t demonstrate all these signs, even when very stressed. Some of these signs suggest low levels of stress, while others are definite warning signs of high anxiety. Understanding where these signs fall on the Fear, Anxiety, and Stress (FAS) spectrum is important.
Dogs2
- Ears pinned back and down
- Furrowed brow
- Lips drawn back with tight commissures
- Head turned away from stressor
- Whale eye (ie, viewing a stressor from the corner of the eye, showing the whites of the eye)
- Dilated pupils
- Tail tucked or held high (may include a stiff wag)
- Crouching and leaning away from stressor
- Raised front paw
- Lateral recumbency with the pelvic limb held up to expose the abdomen
- Yawning
Cats2
- Ears pinned back, sideways, or flattened
- Ears moving fast (vigilant to sounds)
- Dilated pupils
- Head turned away from stressor
- Tail held tightly to the body (tip of the tail may flick)
- Whiskers held perpendicular to the face

2. Create a Low-Stress Veterinary Clinic Environment
We can’t completely eliminate the stress associated with veterinary visits, but we can try to minimize it as much as possible.
Creating a low-stress clinic environment includes arranging the waiting area to allow maximum distance between animals or using barriers that prevent patients from seeing one another. Consider having nervous pets wait outside or in the car rather than in the waiting area.
Many dogs are stressed by being weighed on the scale, so encourage and reward them for stepping on the scale on their own, avoid setting it up in a corner, and ensure it has a non-slip surface.
Try to keep the noise level as low as possible and encourage all team members to speak with quiet and calm voices. Avoid letting doors close loudly, and keep background music off or play pet-friendly tunes at a low volume. Clean frequently not just for hygiene but also to minimize odors—dogs and cats produce alarm pheromones from their paw pads and anal glands when stressed, which can alarm other patients.
Consider using species-specific synthetic pheromones throughout the clinic and asking pet owners to bring their own blankets or towels from home, as the familiar smell is comforting.
Consider placing visuals around the clinic that remind team members about anxiety-related body language and dosages for common previsit anxiolytics.
3. Practice Low-Stress Handling and Create Positive Associations
Low-stress handling is key to making the veterinary visit as stress-free as possible, and it starts with how you greet your patient.
If possible, let dogs approach you. Offer treats if there’s no contraindication, tossing them on the floor if your patient is shy. If you need to approach, do so from the side if possible.
Try to avoid dragging or tipping cats out of their carriers, as this complete loss of control can be very stressful for them. When a cat won’t exit the carrier on its own, remove the top of the carrier. If removing the top is not possible, reach around the cat’s caudal abdomen and hind legs, applying light pressure to encourage it to move forward.
Whenever possible, perform the exam where your patient feels most comfortable. For many dogs, this means conducting the examination on the floor. Cats often prefer to stay in the bottom of their carrier or hide under a towel.
Begin the exam with the least unpleasant step, saving the most unpleasant procedure for last. If possible, give treats throughout the exam to create a positive association. Use smooth, slow movements and continually evaluate how your patient is doing.
Full-body restraint is very stressful for most patients due to unpredictability and loss of control. If possible, use gentle restraint, where the pet is just gently prevented from moving away from you.
When your patient resists restraint for more than 2 or 3 seconds, try a different position or approach. Should they remain uncooperative after 2 or 3 attempts, it’s time to consider other options.
If treatment isn’t urgent, you might want to postpone the procedure and administer anxiolytic medication before the next appointment. When immediate treatment is necessary, consider utilizing injectable sedation.
4. Administer Antianxiety Medications Before Veterinary Visits
There are many drugs that can be used for previsit anxiety relief. Some of the most common drugs are listed in the table below with the dosages listed in Plumb’s™.
| Drug | Class | Dosage |
| Alprazolam | Benzodiazepine | Dog: 0.02 – 0.1 mg/kg PO 30 to 60 minutes before visit Cat: 0.5 – 1 mg/CAT (NOT mg/kg) PO 1 hour before visit |
| Dexmedetomidine oromucosal gel | Alpha-2–adrenergic agonist | Dog: 125 micrograms/m2 (NOT micrograms/kg) OTM 30 to 60 minutes before visit |
| Gabapentin | Anticonvulsant; anxiolytic; neuropathic pain analgesic | Dog: 50 mg/kg PO 2 hours before visit Cat: 50 – 200 mg/CAT (NOT mg/kg) PO 2 hours before visit |
| Trazodone | Serotonin (5-HT2A) antagonist/reuptake inhibitor | Dog: 5 – 7.5 mg/kg PO as needed 90 minutes before visit, up to 19.5 mg/kg daily Cat: 50 mg/CAT (NOT mg/kg) PO 60 to 90 minutes before visit |
These drugs are sometimes combined with one another or with other medications for better effect.
For example, the Chill Protocol, developed at Cummings School of Veterinary Medicine at Tufts University, uses a combination of orally administered medications to manage fearful dogs.
They found that preappointment administration of oral gabapentin with oral melatonin and transmucosal acepromazine significantly decreases stress and increases sedation scores in anxious and fearful dogs during veterinary visits.
While acepromazine is not an anxiolytic agent and should not be used alone, it works synergistically with other sedatives, opioids, and anxiolytics to produce calming effects.
CHILL PROTOCOL
- Gabapentin (20 – 25 mg/kg PO) should be administered the evening before the scheduled appointment.
- A combination of gabapentin (20 – 25 mg/kg PO) and melatonin (small dogs, 0.5 – 1 mg PO; medium dogs, 1 – 3 mg PO; large dogs, 5 mg PO) should be administered at least 1 to 2 hours before the scheduled appointment.
- Acepromazine (0.025 – 0.05 mg/kg OTM) should be administered 30 minutes before the scheduled appointment.
No matter which anxiolytic or combination you choose, read the drug monograph—a comprehensive guide to the drug’s characteristics, usage, and other essential information—before you prescribe to check for any contraindications and to review potential adverse effects.
If your patient is on any other drugs, it’s important to check for potential drug interactions before you prescribe to decrease medication errors and keep your patients safe.
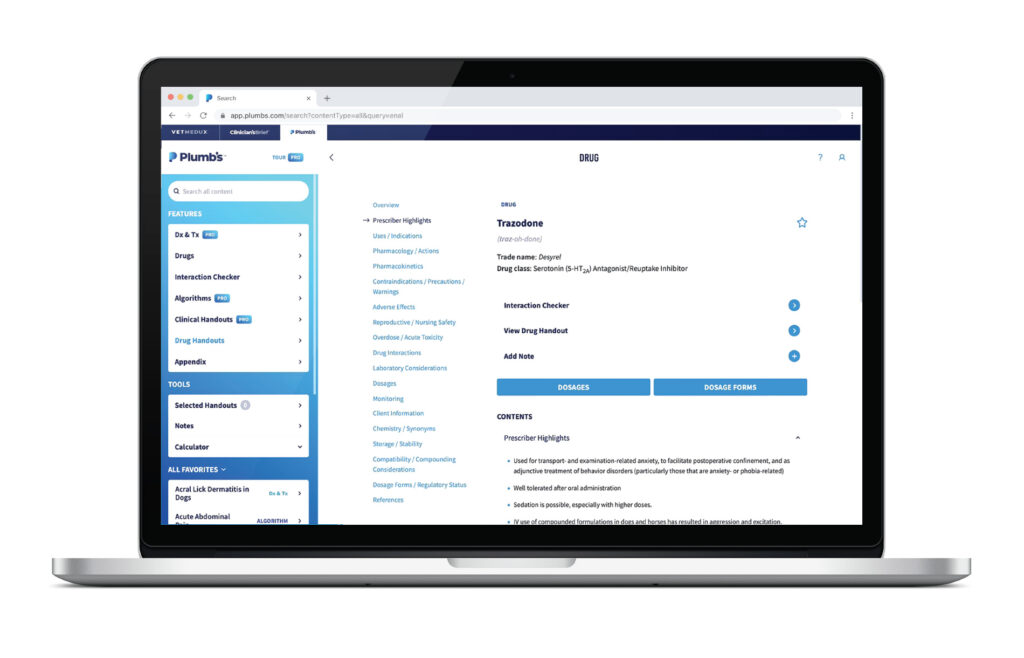
The drug interaction checker in Plumb’s™ contains animal-specific information based on current evidence and is continually reviewed by veterinarians and veterinary pharmacists.
How to Stay on Schedule While Managing Stress and Anxiety
There’s no doubt that managing anxious patients properly and arranging previsit medication takes extra time. Educating clients, determining the medication protocol, calculating dosages, and writing and filling the prescription can add extra time to an appointment.
But there are steps you can take to speed up this process. With Plumb’s™, you can quickly access drug information and calculate dosages from any phone or computer.
Educating your client about the drugs you’re dispensing can be made easier with drug handouts that clearly explain everything a pet owner needs to know about the drugs you prescribe, like side effects, duration of therapy, and what to do if they miss a dose or have pills left over.
Sharing them with clients is easy. Print them in the clinic or email them from a phone or tablet (without revealing your email address). You can even send multiple handouts together.
Although it’s not possible to eliminate all stress for your patients, following these simple steps means you can feel confident you’re helping to minimize their anxiety.
Already subscribed to Plumb’s™? Browse drug handouts or try the interaction checker.
References
- Riemer S, Heritier C, Windschnurer I, Pratsch L, Arhant C, Affenzeller N. A Review on Mitigating Fear and Aggression in Dogs and Cats in a Veterinary Setting. Animals (Basel). 2021;11(1):158. Published 2021 Jan 12. doi:10.3390/ani11010158
- Pike AL. Top 5 clinical signs of stress in dogs & cats during examination. Clinician’s Brief. Last updated December 2022. Accessed May 2024.


